
Editor's note: This article was produced by a student participating in the course J477/577: Strategic Science Communication, a collaboration between the School of Journalism and Communication’s Science Communication Minor program and the Research Communications unit in the Office of the Vice President for Research and Innovation.
Unless they’re gasping for breath at the end of a 5k or doing a deep breathing exercise in a quiet moment before morning coffee, many people take breathing for granted. In fact, you are breathing as you read this sentence and probably aren’t aware of it (though maybe now you are!). But Adrianne Huxtable, an associate professor of human physiology and neuroscience, hopes to bring focus to how the brain controls breathing.
Huxtable’s laboratory investigates the development of neural circuits that control breathing, including how inflammation early in life impacts the nervous system and its regulation of breathing. While most people consider the lungs and airways central to breathing, Huxtable is most interested in the brain’s role coordinating all that activity.
“Part of the reason that I got really interested in the respiratory system,” she says, “was that it’s essential for keeping you alive, and we know surprisingly little about it, which is kind of mind-boggling.”
Scientists know certain regions of the brain are essential for orchestrating breathing, but less is known about how they develop. Understanding this process is essential; the respiratory system is unique because it must function immediately after birth. Around week ten in utero, the human respiratory system becomes rhythmically active. At this point, mothers are supplying oxygen to the growing fetus, but Huxtable and her colleagues believe this early activation—a kind of pseudo-breathing without gas exchange—is key to establishing breathing rhythms, or the daily breaths in and out that the gestating fetus will use for the rest of its life. When born, this system will immediately begin gas exchange, bringing oxygen into the lungs and releasing carbon dioxide.
“There’s no real lag,” Huxtable said of the switch. “You have to start breathing.”
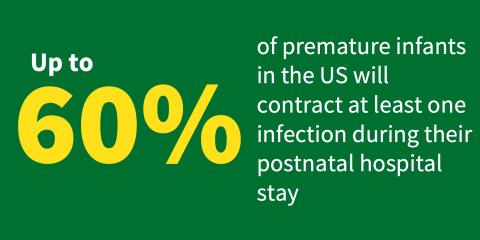
Because the development of this system is so dynamic—both before birth, when rhythms are established, and immediately after birth, when breathing begins—Huxtable’s lab investigates how bacterial and viral infections as infants can impact breathing into adulthood. These infections create inflammation in the body, which occurs whenever the immune system is activated. Inflammation is surprisingly common, as up to 60% of premature infants in the US have at least one infection during their hospital stay, and 27% of all US neonatal deaths within the first week of life are inflammation-related.
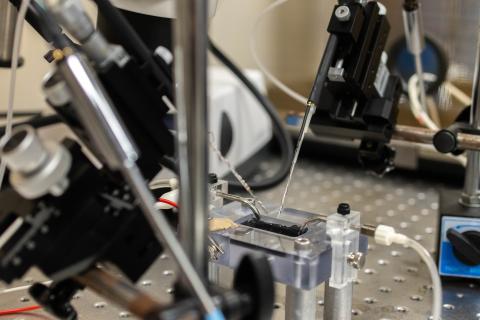
The Huxtable Laboratory uses an animal model to better understand how the nervous system responds to inflammation soon after birth and later in life. The neural circuitry that controls breathing in rodents is very similar to that in humans, making it a powerful model.
“I think the level of understanding we can get using the rodent model is hugely powerful to be able to inform anything that we're going to do in humans,” she said.
By introducing neonatal rodents to bacterial and viral infections and measuring the impact the immune response has on their central nervous systems and breathing, the Huxtable Lab has begun to reveal the intricate connections between inflammation and respiratory control.
Huxtable and her team investigate low-grade inflammation, or the immune response that occurs without triggering symptoms of infection.
“Initially, when we started, I didn’t think it would do much,” she said. “I think what we are just starting to understand is really how systemic inflammation, so inflammation throughout the body, is actually changing the nervous system as a whole.”
Traditional paradigms often frame the central nervous system—the brain and spinal cord—as “immune privileged,” or unaffected by inflammation. Instead, Huxtable’s research, along with many others, demonstrates what she calls “bi-directional communication” between the central nervous system and the immune system to change breathing in adults after this early immune activation, for better or worse.
The main finding from the Huxtable Lab’s research is that respiratory plasticity, or the respiratory system’s ability to learn, adapt, and remember, is impaired by even low-grade inflammation that may impact individuals into their adult lives. Broadly, Huxtable acknowledges these results could improve care for respiratory conditions in adulthood, as today’s treatments are likely not targeting the underlying neurological factors.
In her own research, she looks forward to a new mystery.
“As neuroscientists, we talk a lot about neurons, which are the main signaling cells in the brain, but they actually don't make up the majority of cells in the brain,” she said. “I'm really interested in how these inflammatory challenges are changing cells that are not neurons, because those seem to be the ones that are more responsive.”
Rather than ignoring the automatic action of breathing, Huxtable and her team invite us to see the breath at any age as a miraculous reason to celebrate.
